Patient Information
What is carotid stenosis?
Carotid stenosis refers to narrowing of the carotid artery in the neck. This narrowing has been caused by a build-up of fatty deposits (plaque). There are various reasons for why a carotid artery becomes narrowed, and you can obtain more information about this from your doctor. Most people with carotid artery stenosis have no symptoms (asymptomatic), but the condition can be dangerous if the plaque moves somewhere else and blocks blood flow to the brain. This type of blockage causes around 20% of all strokes.
What is the purpose of the ACST-2 Study?
ACST-2 aims to find out the best way of treating asymptomatic carotid stenosis. All patients in ACST-2 will be on the correct medication, as directed by your doctor. However, because your stenosis is severe, you would also benefit from an operation to open the artery, remove the plaque and thus reduce the risk of having a stroke in the future. The first ACST study (ACST-1) showed that asymptomatic patients who were on medication and had a carotid operation reduced their risk of stroke by half compared to those who were on medication but waited to have an operation when they had symptoms.
Why am I being invited to take part?
Your doctor has given you an information sheet because you may be suitable for both procedures, and you would therefore be eligible to join the ACST-2 study.
Do I have to take part?
It is completely up to you to decide whether or not to take part in the ACST-2 study. If you do choose to take part, you are still free to withdraw at any time and without giving a reason. This will not affect the standard of care you receive.
What will happen to me if I take part in ACST-2?
In this study, we need to compare people who have carotid stenting with those who have carotid endarterectomy. We have summarised each of the procedures below followed by how the treatment would be allocated in the study.
Carotid Artery Stenting (CAS)
This is a procedure where a small, flexible tube called a catheter is placed inside an artery (typically in the groin, wrist or arm). The catheter is moved up to the carotid artery and a small metal-mesh tube stent is then placed to increase blood flow in the areas blocked by plaque. The procedure usually takes around one to two hours to perform, and is often carried out under local anaesthesia. There are some risks associated with having a carotid stent, including a small risk of having a stroke or heart attack (less than 1 in 100) and wound infection (less than 1 in 100). After the procedure, you will need to lie still for about an hour to avoid bleeding from the artery. There is an overnight hospital stay, and most people are able to return home the next day. After the operation, there may be some bruising and soreness for one to two weeks in the area where the catheter was first placed.
Carotid Endarterectomy (CEA)
This involves making a small incision in the neck so that the surgeon can access the carotid artery. The carotid artery is clamped so that the plaque can be removed. The surgeon then stitches the artery, removes the clamp and stops any bleeding. The neck incision is then closed using stiches. The procedure usually takes around one to two hours to perform, and is often carried out under general anaesthesia. There are some risks associated with having a carotid endarterectomy, including a small risk of having a stroke or heart attack (less than 1 in 100) and wound infection (less than 1 in 100).
A small tube may be left on the wound to drain away any blood that might build up after the operation, which is usually removed the following day. After surgery, you may have some discomfort and/or numbness around the neck where the incision was made and there will be a small scar (around 7-10cm). Most people are able to eat and drink a few hours after surgery. There is an overnight hospital stay, and most people are able to return home the next day or the day after. Some patients can have a hoarse voice for a few weeks after the surgery.
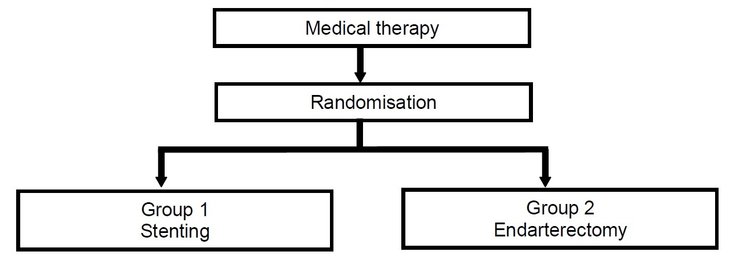
Treatment allocation
The best way to compare these two treatments is to have similar groups of patients having either a stent or endarterectomy. Everyone who agrees to take part in this research study will be allocated to either stent or endarterectomy. The only way to make sure that the groups of patients are as similar as possible is to have the allocation decided by chance: a process called randomisation. This means that you will have an equal chance of having either stenting or surgery. This process ensures that the treatments within the study are compared fairly. Whichever treatment you are allocated to, you will be treated with the best possible care and the doctor treating you will be experienced in the technique.
If you do decide to take part you will be given an information sheet to keep and asked to sign a consent form. The research nurse or doctor will ring the research centre in Oxford, where your treatment will be identified through randomisation – you will have an equal chance of having a stent or endarterectomy. It is important for the study that you only agree to take part if you believe you would be prepared to accept either treatment. The research nurse will tell you the treatment straight away. The operation will then be done as soon as possible (ideally within the first month after the treatment is allocated).
Follow-up
After you have the operation, you will be seen by a hospital doctor about one month later to find out about your general health. Then, every year for at least five years, the study team will send you a short questionnaire to find out about your experiences of the operation and any problems you may have had. Your normal medical care will not be affected by taking part in the study.